Catastrophic Plans: Healthcare Exchange
The Patient Protection and Affordable Care Act, more commonly known as ObamaCare, begins January 2014 has a provision for Catastrophic Coverage -this coverage is only for a specific group of Americans.
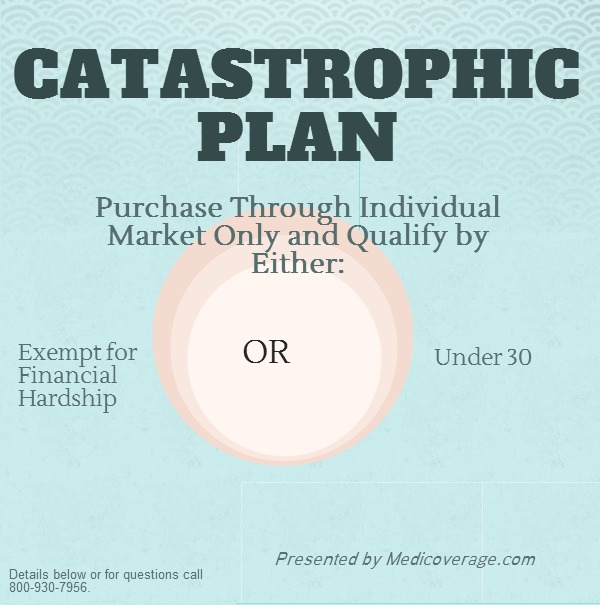
Who is eligible for Catastrophic Coverage?
- Persons under 30 OR
- Hardship exemption from traditional Exchange Plans AND
- Purchasing a plan through the individual market only
Catastrophic Plan Overview
*Approximately $6,350 for 2014
What are the other Healthcare Exchange Plans?
The standardized plans are Bronze, Silver, Gold, and Platinum. These plans must include essential health benefits before you meet your deductible or out-of-pocket max, certain plans and individuals qualify for federal premium subsidies and federal cost-sharing subsidies, and these plans are defined by the percentage of cost-sharing from 10-40%. Click here to compare Bronze, Silver, Gold, and Platinum plans side by side. For help signing up with any of the Healthcare Exchange metal plans call 800-930-7956.
Next Steps
For any further questions about Catastrophic Plans in your state contact Medicoverage.

Comments and Questions
Click to leave a CommentComment from Teresa Garcia on January 21, 2016
Yes, my adult disabled son who has Denti-cal needs to have 4 crowns done and needs a partial upper denture. Denti-cal pays for prefabricated crowns and I have called all of the
dentists that Denti-cal said to call and they are not doing the prefabricated crowns anymore.
I need to get my son dental insurance to get this work done asap as he is an uncontrolled diabetic and is on insulin and is at high risk for infections. I prefer to get him into a PPO plan so he can see any dentist. His dentist submitted a pre-authorization for his treatment plan, however, Denti-cal denied all claims. Please advise. Sincerely, Teresa Garcia
MEDICOVERAGE AGENT RESPONSE
Teresa,
We definitely know how frustrating it can be to not get the care that is necessary. You can get a dental quote here, and then you’ll be able to see how each plan covers crowns. If you need further help call 800-930-7956, and we’d be happy to find a plan for your son.
-Chris from